Face, Mid-face, Cheek, Eyelid and Orbit Anatomy

Understanding Facial Anatomy
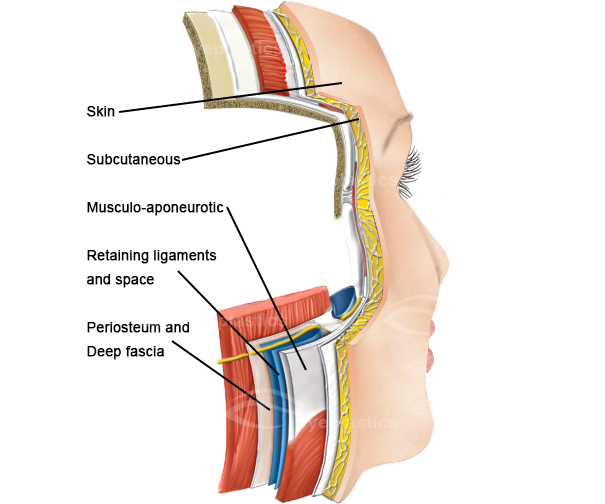
- Your face is made up of layers of tissues varying in texture and consistency. These tissue layers overlie the bony skull, which provides the support for and structure of your face. From a cosmetic surgeon’s standpoint, your face is made up of the following components: skin, fat, superficial musculoaponeurotic system (SMAS), platysma muscle, Erb’s point (containing important nerves), deep cervical fascia and the retaining ligaments of the face. Mastering the art of tweaking these components in the correct proportion and in an aesthetically pleasing manor is the surgeon’s delight and goal, the reward being the facial iimprovementthat you desire.
- The thickness of skin overlying your face is variable - your eyelids have the thinnest skin while your cheeks and forehead are covered by a thicker skin. Facial skin is repeatedly exposed to the sun and elements. This skin is also affected by aging, resulting in loss of elasticity and the development of rhytids or wrinkles. The skin consists of two main layers - the inner layer called dermis and the outer layer called epidermis. Our epidermis is what everyone sees!
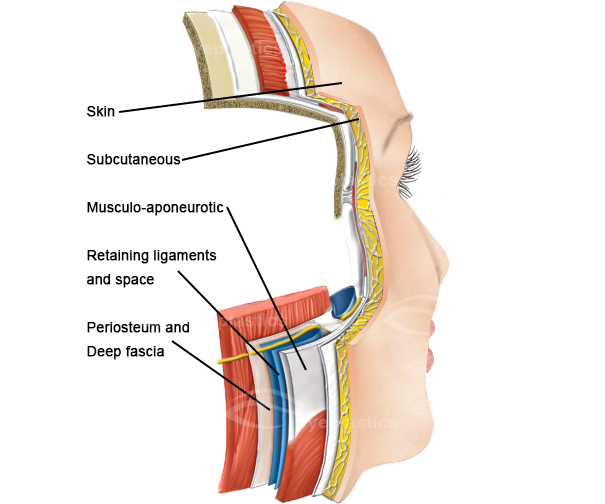
- Fat is one of the most important components of your face and lies just beneath your skin, i.e. subcutaneous fat. It consists of lobules partitioned by fibrous septa which connect the inner layer of the skin, the dermis, to the superficial fascia just beneath the fat. The distribution of fat in the face is variable, with a major portion deposited right beneath your cheek as the malar fat pad. It is also found below the eyes, lateral to your nose, and in front of your ears. Fat accentuates your cheek bones nicely. The malar fat pad is propped up by connections to the orbitomalar ligament, the superficial musculoaponeurotic system (SMAS), underlying soft tissue, and bone. With age, the malar fat pad shrinks, causing the cheeks to droop towards the crease between your nose and lips. This drop of cheek tissue results in a deeper fold and shadow-- a definite sign of aging.
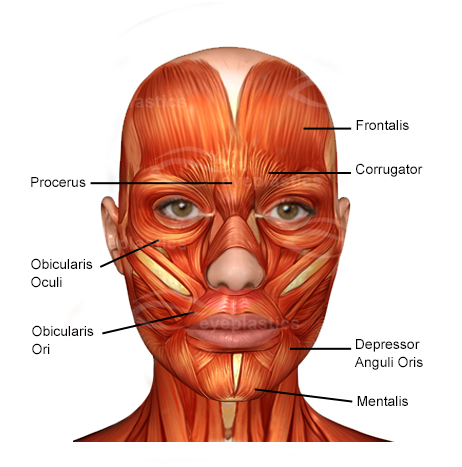
- The SMAS or superficial musculoaponeurotic system covers and connects the muscles of facial expression to the deeper layers of your face. It lies beneath the fat layer of your skin and provides definition to your facial expressions. The SMAS is a thin layer of connective tissue that lies attached closely with the platysma muscle, frontalis muscle, galea and superficial temporal fascia. It is also closely attached to the superficial muscles of facial expression (including the orbicularis muscle), pre-orbicularis fat and the malar fat pad. The SMAS is attached to bone at the infraorbital rim, zygoma, and the mandible.
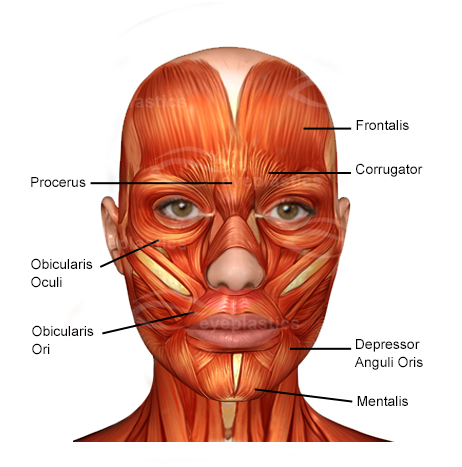
- The Platysma is a thin, flat muscle that begins in the chest just in front of your collar bone, the clavicle, moving up towards the face and covering the front and sides of the neck. It eventually attaches to your jaw bone and skin, then merges with several muscles and continues as the SMAS over the parotid (salivary) gland and cheek. Both sides of the Platysma merge at the midline just below your jaw line. As one ages, the platysma muscle becomes loosely attached to the underlying structures resulting in vertical banding and bowing under the chin.
- The Deep Cervical Fascia is a connective tissue in the neck that covers and protects the muscles, nerves, blood vessels and glands of the face. Surgery deep to the deep cervical fascia can result in injury to the facial nerve, which is the primary nerve supply to the face. Damage to any of its five branches could cause weakness of the muscles supplied by that particular branch. Utmost care must be taken to avoid injury to the facial nerve or its branches.
- Erb’s point lies vertically below the ear canal just behind the sternocleidomastoid muscle and represents the point of emergence of several nerves that provide sensation to the neck and lower face. It lies just over the sternocleidomastoid muscle. Its largest branch, the greater auricular nerve emerges 6.5 cm below the ear canal and provides sensations to the lower portion of the ear and area just behind the ear. Hence, it is important to meticulously dissect this area to avoid damaging any of these nerves.
- Retaining ligaments or tendons provide support to the soft tissues of the face and also provide points for movement of muscles of facial expression. The retaining ligaments important during rhytidectomy surgery are:
- Osteocutaneous ligaments: connecting from bone to the inner layer of the skin (the dermis). Zygomatic and orbito-malar ligaments suspend the soft tissue of the malar region. The submental crease is formed by the mandibular osteocutaneous ligament.
- Fascial-cutaneous ligaments bind the superficial and deep fascial layers of the face.
.jpg)
Underneath the skin, along with the subcutaneous tissue is a thin layer of fat. However, the amount of fat is negligible when compared to other parts of the body. Typically, subcutaneous tissue is absent at points where the skin is attached directly to underlying ligaments such as the medial and lateral palpable ligaments. The skin and subcutaneous tissue can be subject to certain clinical conditions such as dermatochalasis and blepharochalasis.
Submuscular areolar tissue
- This is a loose connective tissue that lies beneath the orbicularis oculi muscle. It can form an anatomical plane that divide the eyelid into a front (anterior) and back (posterior) portion. The fibres of the levator aponeurosis then passed through this plane in the upper eyelid. A small portion of these fibres contribute towards the development of the upper eyelid crease. Similarly, in the lower eyelid, the fibres of the orbitomalar ligament passed through this plane.
- If this anatomical plane were to be tracked towards the eyebrow area, the retro-orbicularis oculi fat will be traversed. If the plane were to be tracked towards the cheek, the sub-orbicularis oculi fat would be traversed.
Orbicularis retaining ligament
- Also called the orbital retaining septum or orbitomalar ligament, this ligament attaches the orbicularis oculi muscle to the lower rim of the orbit. It is weak in its central aspect, and a lot stronger in the lower-outer aspect. When traced laterally, it is contiguous with tissue that is formed by fusion of the outer part of the orbicularis oculi and the deeper periosteum and temporalis fascia. This fusion is called the orbital thickening. This orbital thickening covers the frontal process of the zygomatic bone.
- As one gets older, the orbicularis retaining ligament tends to get thinned out and stretched, with these changes more prominent in the central aspect. When excised along with the orbital thickening, it results in full release of the superficial fascia that lines the orbital rim.
Upper lid retractors
- The upper lid retractors are a group of muscles whose main function is the keep the upper eyelid elevated. The muscle that forms a part of this is called the levator palpebrae superioris (LPS). This muscle originates from the bottom aspect of the lesser wing of the sphenoid bone located within the skull. It consists of 2 heads - the levator muscle and the superior rectus muscle. They are joined together by fibrous tissue. From its origin, the LPS traverses horizontally forward for about 40mm, ending in an aponeurosis that is around 10mm posterior to the orbital septum. It then takes a more vertical course toward the Whitnall ligament (superior transverse ligament).
- The Whitnall ligament is similar to the previously described orbital fascia and lies in close proximity to the aponeurotic and muscular junction of the LPS. It extends around the upper margin of the orbit in a plane that lies between the lacrimal gland fascia and the trochlea. The LPS varies in thickness, and is relatively thin in areas between the upper orbital rim and the Whitnall ligament.
- When traced inwards and outwards, the LPS aponeurosis forms ‘horns’ called medial and lateral horns. The lateral horn runs through the lacrimal gland, dividing it into 2 lobes - the palpebral lobe and the orbital lobe. Having done this, it goes on to attach to the lateral retinaculum located at the lateral orbital tubercle. On the other hand, the medial horn has a more direct course and is fixed to the posterior lacrimal crest.
- The aponeurosis eventually reaches the border of the superior tarsal plate having fused originally with the orbital septum. At the bottom end of this fusion, a small part of the aponeurosis attaches to the lower aspect of the anterior part of the tarsal plate. One part of this fusion extends forwards to insert into the pretarsal orbicularis oculi muscle and skin, resulting in the formation of the skin crease in the upper eyelid.
Fat Pads
- There are a number of different fat pads that are present within and around the eyelid. One layer of fat called the pre-aponeurotic fat is found right behind the orbital septum and in front of the levator aponeurosis. Also within the upper eyelid are two more areas that contain fat pads that are centrally and medially (towards the nose) located. The medial fat pad is pale yellow in colour and lies in front of the levator aponeurosis.
- On the other hand, the central pad of fat is broader and yellow in colour. As it travels outwards, it wraps around the inner aspect of the lacrimal gland. The lacrimal gland can be clearly seen and differentiated from this fat by its pink colour and lobulated structure. The lacrimal gland is positioned just posterior to the orbital margin but could prolapse slightly making it more prominent when the eye is examined.
- While the above described the fat pads within the upper eyelid, the lower eyelid fat pads are slightly different in structure. The inferior oblique muscle separates the central fat pad from the dinner medial fat pad. There is a small amount of fat that lies in front of the inferior oblique muscle as well. The inferior oblique muscle originates from a small indentation in the lower border of the orbital floor, moving behind the orbital margin and at the upper aspect of the nasal lacrimal canal. It passes underneath the inferior rectus muscle and through the Tenon capsule, ultimately inserting at the point close to the macula of the eye. This rather winding course of the inferior oblique muscle makes it vulnerable to injury during this section of the fat pads around the eyelid and eye.
Blood supply
- The eyelids are supplied by branches of the internal and external carotid arteries. The ophthalmic artery branches off the internal carotid artery and supplies different parts of the eyelid. At the inner part of the upper eyelid, the ophthalmic artery splits into two and traverses outwards the supply both the upper and the lower eyelid. The branch that supplies the lower eyelid is in fact a branch that arises from the superior marginal vessel (that supplies the upper eyelid). The superior and inferior marginal vessels that arise from the ophthalmic artery together form the marginal arcade.
- The marginal arcade arteries are located at the front of the tarsus, 4 mm from the upper eyelid and 2 mm from the lower eyelid margin each. The superior marginal arcade gives rise to a peripheral arcade that runs in front of the Muller muscle, giving it a superficial plane and making it prone to injury during eyelid surgery. The peripheral arcade in the lower eyelid is often rudimentary.
- Another branch of the internal carotid artery is the lacrimal artery that passes through the orbital septum along each eyelid and ultimately joins the marginal arcade.
- While the above described the branches of the internal carotid artery, the external carotid artery supplies the eyelids as branches of the facial artery, infraorbital artery and the superficial temporal artery. Each of these pride branches that anastomosis with other arteries on the face. For example, the branch of the superficial temporal artery that supplies the eyelids joins with the zygomatic branch and transverse facial branch.
.png)

.jpg)